Scientists Uncover a Possible Genetic Tie Between Brain Blood Vessel Damage and Alzheimer's Disease
High blood pressure, diabetes, heart disease, and obesity are risk factors that may raise a person’s chances of experiencing the type of brain blood vessel damage that often underlies strokes and other neurovascular disorders. A gene called FMNL2 may play a critical role in linking these factors to the brain damage seen in some cases of Alzheimer’s disease, according to an NIA-funded study by Columbia University researchers.
FMNL2 encodes a protein that is known to help build the structures (known as cytoskeletons) found in cells throughout the body. The findings, published in Acta Neuropathologica, suggest that in Alzheimer’s, FMNL2 helps reshape a protective barrier between the brain and blood vessels, and that this process may speed the removal of damaging proteins.
For decades, some scientists have strongly suspected that Alzheimer’s is, in many ways, a blood vessel disorder. About 70% of patients show signs of the types of brain blood vessel damage often observed after strokes, and many of the risk factors that raise the chances of developing heart disease do the same for Alzheimer’s. In this new study, the researchers searched for clues as to how these factors may interact with one’s genes to elevate the chances of experiencing Alzheimer’s.
To this end, they analyzed the health and genomic data of 14,669 individuals of diverse racial and ethnic backgrounds who participated in several aging and Alzheimer’s studies conducted across the United States. The average age of the participants was approximately 80 years old, and nearly 38% had been diagnosed with Alzheimer’s.
First, the researchers used four factors to calculate a cerebrovascular risk score: diabetes; heart disease; obesity; and hypertension, which is sometimes called high blood pressure. Multiple previous studies have indicated these factors are often associated with experiencing strokes and other cerebrovascular diseases, as well as with Alzheimer’s.
In this study, about 70% of the participants had hypertension, 33% had heart disease, and 21% had diabetes. Based on body mass index scores, the average participant could also be classified as obese. Hypertension and diabetes were both highly correlated with and strongly influenced the Alzheimer’s risk scores.
Next, the team used several advanced data analysis techniques to test how the risk factors may combine with each gene on an individual’s chromosomes. They consistently found that the FMNL2 gene interacted the most with the cerebrovascular risk factors to raise Alzheimer’s risk.
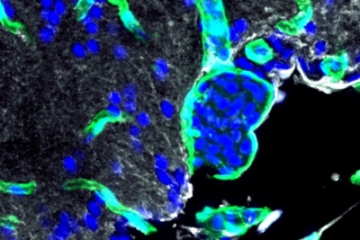
Further support for this idea evolved when the scientists examined autopsied brain tissue. The brains of Alzheimer’s patients had high levels of the FMNL2 proteins surrounding blood vessels. The proteins appeared concentrated in astrocytes, which are star-shaped brain cells that line the blood-brain barrier. The blood-brain barrier prevents pathogens and toxins, which circulate throughout the blood system, from entering the brain.
In the brains of people who had died with Alzheimer’s, some astrocytes appeared “reactive” — in other words, in a diseased state — and detached from the barrier. The researchers observed these findings regardless of whether the person had been diagnosed with atherosclerosis, a disease that hardens blood vessels. In contrast, in the brains of age-matched control subjects without Alzheimer’s, FML2 proteins appeared sparsely, the astrocytes looked healthy, and the blood-brain barriers were intact.
The researchers saw similar signs of damage in the brains of mice that had been genetically engineered to mimic certain aspects of Alzheimer’s, supporting the idea that these changes may be a common reaction to the disease.
Finally, experiments in zebrafish suggested that the reaction may be triggered by the accumulation of beta-amyloid, a protein thought to play a key role in damaging the brain during Alzheimer’s. Injections of beta-amyloid resulted in high levels of FMNL2 protein appearing in astrocytes, many of which had detached from the blood-brain barrier.
Interestingly, these changes may help the brain remove beta-amyloid. For instance, genetically turning off FMNL2 gene activity in astrocytes resulted in higher levels of injected beta-amyloid accumulation in zebrafish brains.
Overall, the results suggest that FMNL2 and other genes involved with blood-brain-barrier maintenance may be important candidates for developing new treatments that can counteract the damage caused by Alzheimer’s, especially in those who experience cerebrovascular risk factors.
Source: National Institute on Aging


